In 2018, the Defense Health Agency (DHA) will begin making major reforms to the Military Health System (MHS) and changes to the organizational structure of several Department of Defense (DoD) medical research programs. We’re following these R&D transitions and summarized below are a few of the changes to the Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury, Defense and Veterans Brain Injury Center and Deployment Health Clinical Center, National Center for Telehealth and Technology, and DoD HIV/AIDS Prevention Program.
The Defense Health Agency (DHA) is a joint integrated  Combat Support Agency that enables the Army, Navy, and Air Force medical services to provide a medically ready force and ready medical force to Combatant Commands in both peacetime and wartime. The DHA supports the delivery of integrated, affordable, and high-quality health services to Military Health System (MHS) beneficiaries and is responsible for driving greater integration of clinical and business processes across the MHS by:
Combat Support Agency that enables the Army, Navy, and Air Force medical services to provide a medically ready force and ready medical force to Combatant Commands in both peacetime and wartime. The DHA supports the delivery of integrated, affordable, and high-quality health services to Military Health System (MHS) beneficiaries and is responsible for driving greater integration of clinical and business processes across the MHS by:
- Integrating shared services with common measurement of outcomes;
- Enabling rapid adoption of proven practices, helping reduce unwanted variation, and improving the coordination of care across time and treatment venues;
- Exercising management responsibility for joint shared services and the TRICARE Health Plan; and
- Acting as the market manager for the National Capital Region (NCR) enhanced Multi-Service Market.
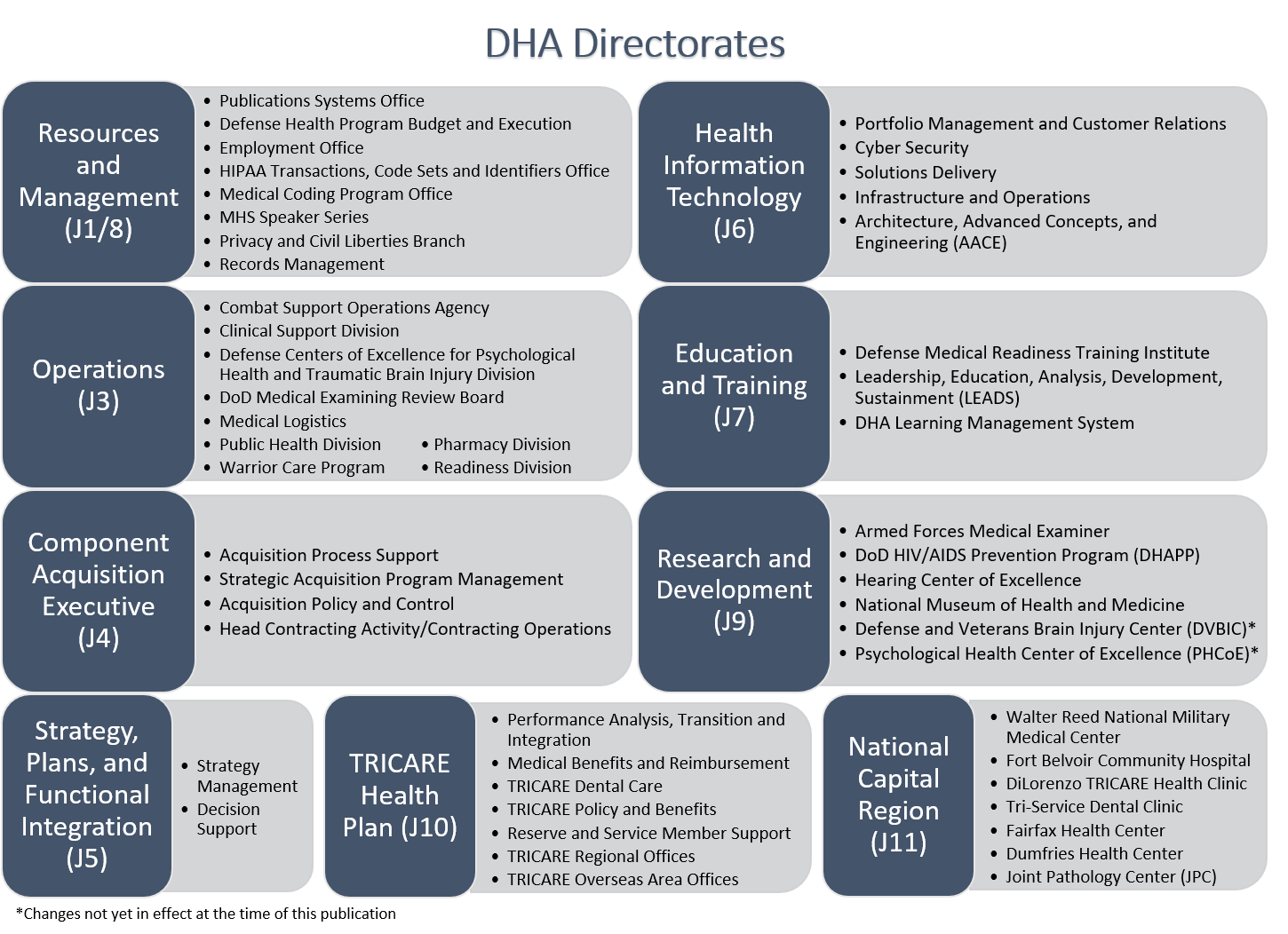
The DHA Directorates and their subordinate centers and offices are listed in accordance with the new changes in the figure below.
Military Health System (MHS)
The Military Health System (MHS) is a complex system led  by the office of the Assistant Secretary of Defense for Health Affairs that weaves together:
by the office of the Assistant Secretary of Defense for Health Affairs that weaves together:
- Health care delivery;
- Medical education;
- Public health;
- Private sector partnerships; and
- Cutting-edge medical research and development.
Reforms to MHS that the DHA has undertaken include creating a more globally integrated health system, driving enterprise-wide shared services with standardized clinical and business processes that produce better health and better health care, and implementing future-oriented strategies to create a better, stronger, and more relevant medical force.
FY18 DHA/MHS Changes and Realignment of DoD Centers and Programs
The FY17 National Defense Authorization Act (NDAA) prescribed major reforms to the TRICARE benefit, MHS organization, and authorities. It also directs changes to how on-base hospitals, clinics, and staff are organized and operate so military providers can care for more patients.
In coordination with these changes, the DHA is taking additional actions to optimize the MHS organization. These realignments and agency changes are part of an overall effort to address the DHA quadruple aim: to provide better health, better care, lower costs, and improve military readiness.
The Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury (DCoE)
The Defense Centers of Excellence for Psychological Health and Traumatic Brain Injury (DCoE) has provided the MHS with current and emerging psychological health and traumatic brain injury (TBI) clinical and education information. The DCoE has operated as a division of the DHA Operations Directorate. However, as of November 1, 2017, the DCoE realigned under the DHA as part of the ongoing MHS transformation. According to the acting DCoE director, “We are consolidating our efforts and nesting our expertise to manage programs, develop resources, and execute research more effectively.” Previously, DCoE consisted of a headquarters, two congressionally designated centers of excellence (the Defense and Veterans Brain Injury Center and the Deployment Health Clinical Center), and the National Center for Telehealth and Technology (T2).
and Traumatic Brain Injury (DCoE) has provided the MHS with current and emerging psychological health and traumatic brain injury (TBI) clinical and education information. The DCoE has operated as a division of the DHA Operations Directorate. However, as of November 1, 2017, the DCoE realigned under the DHA as part of the ongoing MHS transformation. According to the acting DCoE director, “We are consolidating our efforts and nesting our expertise to manage programs, develop resources, and execute research more effectively.” Previously, DCoE consisted of a headquarters, two congressionally designated centers of excellence (the Defense and Veterans Brain Injury Center and the Deployment Health Clinical Center), and the National Center for Telehealth and Technology (T2).
DHA will retire the DCoE brand, but the staff will continue its work on valued programs and initiatives across the agency. DCoE website and social media content will transition to health.mil and MHS social media. The continued missions of the DCoE and its components as part of the new DHA structure will optimize operations at the agency by uniting research assets and nesting DHA centers of excellence in one location.
Defense and Veterans Brain Injury Center (DVBIC)
The Defense and Veterans Brain Injury Center’s (DVBIC)  mission is to serve active-duty military, their beneficiaries, and Veterans with TBI through state-of-the-science clinical care, innovative clinical research initiatives and educational programs, and support for force protection services. The DVBIC is responsible for the following tasks:
mission is to serve active-duty military, their beneficiaries, and Veterans with TBI through state-of-the-science clinical care, innovative clinical research initiatives and educational programs, and support for force protection services. The DVBIC is responsible for the following tasks:
- Creation and maintenance of a TBI surveillance database;
- Service compliance for pre-deployment neurocognitive testing;
- Creation and distribution of the Family Caregiver Curriculum;
- Design and execution of a 15-year longitudinal study of the effects of TBI in Operations Iraqi and Enduring Freedom (OIF/OEF) service members and their families; and
- Design and completion of independent head to head study to evaluate the reliability and validity of computerized neurocognitive tests.
The DVBIC will join the DHA Research and Development Directorate (J9).
The Deployment Health Clinical Center (DHCC)/ Psychological Health Center of Excellence (PHCoE)
DHCC has been renamed the Psychological Health Center of  Excellence (PHCoE). The PHCoE’s mission is to improve the lives of our nation’s service members, Veterans, and their families by advancing excellence in psychological health care and prevention of psychological health disorders. Major areas of focus are to:
Excellence (PHCoE). The PHCoE’s mission is to improve the lives of our nation’s service members, Veterans, and their families by advancing excellence in psychological health care and prevention of psychological health disorders. Major areas of focus are to:
- Develop and implement evidence-based treatments and clinical support tools to improve psychological health specialty care;
- Promote a culture of support for psychological health by improving psychological health literacy, developing patient empowerment tools, encouraging help-seeking behavior and reducing barriers to care;
- Conduct an integrated portfolio of psychological health research to improve the system of care including identifying gaps and prioritizing needs with a goal of translating research into clinical practice and improving patient outcomes;
- Integrate behavioral health into primary care to improve early identification and treatment of psychological health concerns; and
- Provide program monitoring and evaluation services, and develop metrics and measures to inform performance, outcomes, and health care utilization.
Along with DVBIC, PHCoE will also join the DHA Research and Development Directorate (J9). The PHCoE has taken over responsibility of overseeing the Department of Defense (DoD) Suicide Event Report (DoDSER) previously managed by T2. The DoDSER system standardizes suicide surveillance efforts across the Air Force, Army, Marine Corps, and Navy to support the DoD’s suicide prevention mission. The PHoCE is also now overseeing a couple of DCoE’s previous programs: the inTransition program, a free voluntary program with coaches who provide psychological health care support to service members, veterans, and their health care providers during times of transition; and the 24/7 Outreach Center.
The National Center for Telehealth and Technology (T2)
The National Center for Telehealth Technology (T2) will be  integrated into several other components of the DHA. Although the DHA will retire the T2 brand, staff will continue their unique mission of leading the innovation of mobile health and telehealth solutions to deliver psychological health and TBI care and support to our nation’s warfighters, Veterans, and their families.
integrated into several other components of the DHA. Although the DHA will retire the T2 brand, staff will continue their unique mission of leading the innovation of mobile health and telehealth solutions to deliver psychological health and TBI care and support to our nation’s warfighters, Veterans, and their families.
The previous T2 mobile health program, telehealth program, and training program will comprise the new Connected Health Branch under the DHA Clinical Support Division, Operations Directorate (J3). Technology efforts will transition to the Web and Mobile Technology Program Management Office in the DHA Solution Delivery Division, Health Information Technology Directorate (J6). As mentioned above, T2’s previous DoDSER program is now overseen by the PHCoE.
DoD HIV/AIDS Prevention Program (DHAPP)
Oversight of the DoD HIV/AIDS Prevention Program (DHAPP) will be transferred over to DHA from Navy Medicine. DHAPP was established to help contain the global health threat posed by the HIV pandemic. DHAPP’s mission is to assist foreign militaries develop HIV control programs in support of global health security and DoD security cooperation efforts. DHA oversight of DHAPP will streamline interagency collaboration and enhance DHA’s global health engagement capabilities and mission.
will be transferred over to DHA from Navy Medicine. DHAPP was established to help contain the global health threat posed by the HIV pandemic. DHAPP’s mission is to assist foreign militaries develop HIV control programs in support of global health security and DoD security cooperation efforts. DHA oversight of DHAPP will streamline interagency collaboration and enhance DHA’s global health engagement capabilities and mission.
What Now?
If your small business concern (SBC) is developing an innovative dual-use technology in one of our 2018 technology focus areas (cancer therapeutics, orthopaedic trauma tech, traumatic brain injury, and sensors/internet of things), we may be able to assist by:
- Determining whether your technology is currently a capability interest to the DoD;
- Identifying non-dilutive funding opportunities that are available for your SBC to apply;
- Identifying DoD subject matter experts for collaboration via CRADAs;
- Prioritizing the non-dilutive funding application to pursue near-term, and most importantly why; and
- Assisting with DoD-specific narrative/terminology development for your submission package.
If you would like more information on how Tier Seven can assist your small business with identifying, connecting and collaborating via CRADAs with other DoD researchers, please contact us.
23 Jan
2018
